It goes without saying that there isn’t a “one size fits all” option for mental health treatment. There are a wide variety of therapies, medications, settings and regimens that can be tailored to fit a person’s needs. For some, mental health issues are managed well with regular talk therapy sessions, while others with more severe mental health challenges may need an acute inpatient stay at a psychiatric hospital unit followed up with a gradual step down of intensive therapies.
There’s a spectrum of mental health care levels available to you, and today we’ll be taking a closer look at an option for those who may need more than regular outpatient clinic visits: intensive outpatient programs.
What is an intensive outpatient program (IOP)?
An intensive outpatient program (IOP) is a structured treatment program that provides mental health services such as therapy and care for people who require a more intensive treatment plan but don’t require the constant supervision provided during a stay at a residential psychiatric facility – as is common with inpatient treatment. This structure helps to provide a holistic approach to care while allowing those in treatment to carry on with their daily lives.
IOPs are commonly used for moderate to severe mental health issues like depression, anxiety disorders, substance abuse treatment, eating disorders, or post-traumatic stress disorder (PTSD). Typically, an IOP lasts eight to 12 weeks but can be modified to fit the individual needs of a patient.
What therapies and treatments are used during an IOP?
One of the benefits of an IOP is that it allows for a more comprehensive approach to mental health care. An IOP can include a variety of therapies, medication management, and aftercare planning. The specific treatments and therapies used will vary depending on individual needs, but often include some combination of the following:
Intake Assessments
Typically, an IOP includes a mental health assessment to diagnose mental health conditions, identify potentially overlapping conditions, and establish a baseline for monitoring progress.
Individual Therapy Sessions
Regular one on one therapy sessions are a foundational element of an IOP. These are used to address specific mental health concerns, probe into underlying issues, and develop personalized treatment goals. The format of these sessions can vary between treatment centers, but approaches like cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT) and client-centered therapy are commonly used.
Group therapy
Another core therapeutic approach during an IOP is that group therapy sessions offer an opportunity to explore mental health issues with a group facing similar challenges. This can help provide new perspectives, greater accountability, camaraderie, and a feeling of support from others in a similar position as well as introduce new coping strategies.
“Group therapy is an important element of an IOP because it encourages clients to practice vulnerability by sharing with others as well as giving and receiving feedback,” says Dr. Robyn Janssen, Senior Director of National Clinical Programs at Ellie Mental Health. “The benefits of this approach include the development of communication and social skills, reducing feelings of isolation, having opportunities to learn from others, and growing a sense of belonging or relatability through sharing common experiences.”
Medication management
An IOP provides an ideal opportunity to get prescription medications fine-tuned with the help of a healthcare provider during regular check-ins. This can help patients minimize unwanted side effects and find the right dosage and medication combinations, in turn making it easier to stick to a medication regimen.
Holistic interventions
While therapy and medication-related efforts during an IOP may immediately come to mind, these programs provide an opportunity to build healthy habits with holistic early intervention services. This can come in a variety of forms, whether that’s developing an effective meditation routine, finding ways to improve your overall nutrition, encouraging mindfulness activities, or identifying positive self-care opportunities throughout your day.
“These holistic efforts supplement therapy sessions by being practical skills you can use at home or work when needed,” Dr. Janssen explains.
Education
In an IOP, intensive outpatient treatment will also typically include several opportunities for educating patients and their loved ones. Information about mental health conditions, symptoms, treatment options, and strategies for managing the condition is provided. These education efforts can help reduce stigma, develop additional buy-in for treatment plans, and empower patients and families.
“It is incredibly important to provide education to both clients and families during an IOP,” Dr. Janssen says. “When families know what is helpful, they can then encourage the client to utilize these coping skills at home–which helps them maintain the progress they’ve made.”
Case management, relapse prevention, and aftercare planning
The road to keeping acute mental health challenges managed is long and ongoing and certainly doesn’t stop after the completion of an IOP. Case management, relapse prevention, and aftercare planning efforts are an important part of setting the stage for those next steps – and this could also include residential treatment programs. Case managers will help you get connected with providers, schedule appointments andnavigate the complexities of care and insurance coverage. Dr. Janssen shares these efforts are an important piece of the puzzle as they help support the progress made by clients and provide a structured path back to a less-intensive outpatient level of care.
With this holistic mix of services, an IOP provides a comprehensive toolkit for getting on track with long-term mental health treatment.
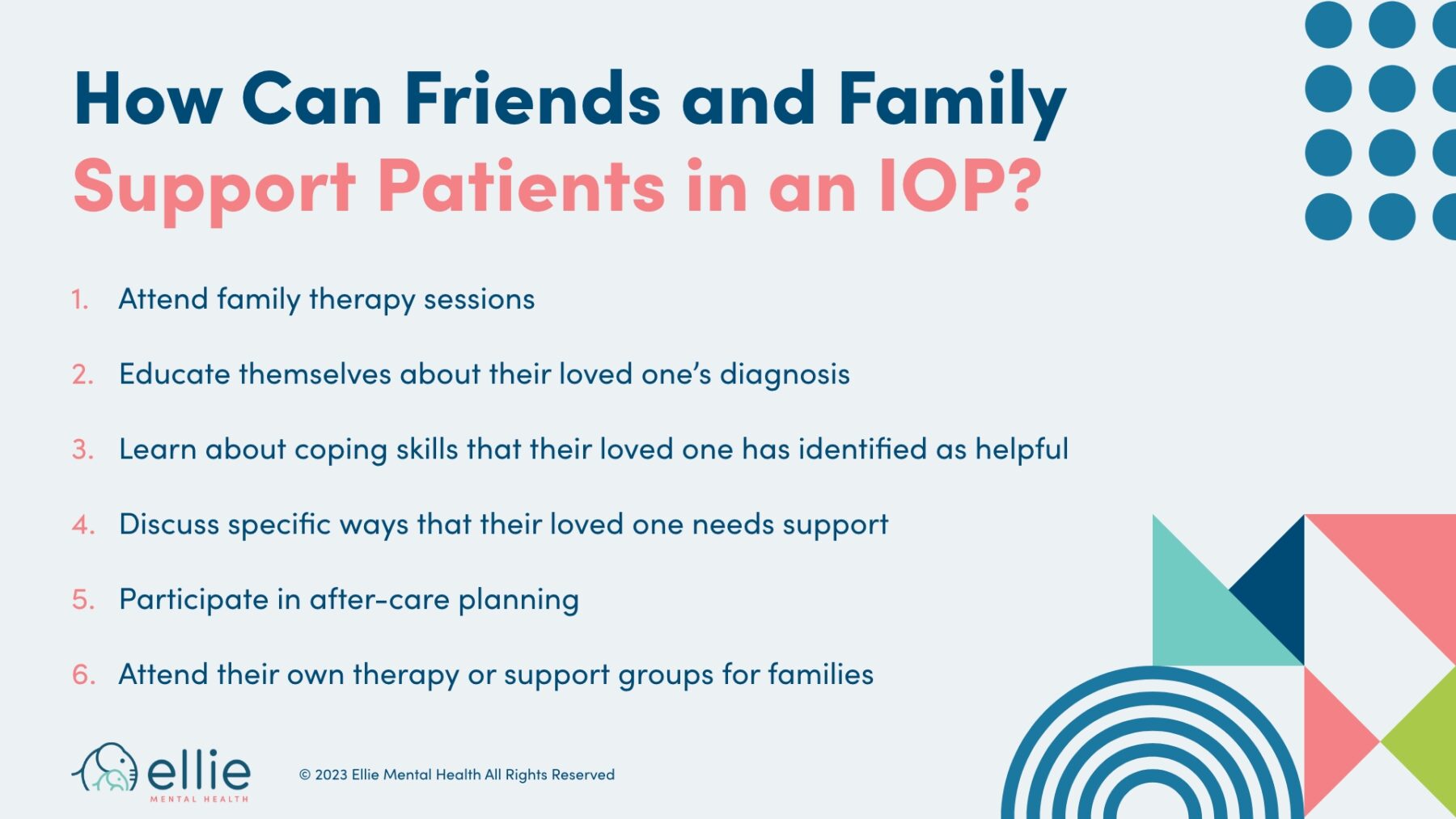
How can friends and family support patients in an IOP?
Support is an important factor for anyone undergoing a challenging time in their life, and friends and family members should expect to take an active role during–and after–their loved one enters an IOP.
While in an IOP, friends and family members may be asked to join in educational sessions as well as family therapy sessions.
“In family therapy sessions, friends and family members can receive psycho-education about the client’s diagnosis, learn about coping skills that the client identified as helpful, and learn and discuss specific ways they can support their loved one,” Dr. Janssen says.
With aftercare planning and an established and invested support group, the transition to life post-IOP becomes more manageable. This can help with relapse prevention and keeping on track with treatment options.
Is an intensive outpatient program right for me?
Entering into an IOP is a substantial undertaking, so how do you know if this step is right for you or others in your life? This is a question that’s ultimately best answered through discussion between a patient, their family and their mental health provider. That said, there are some general criteria that can help you determine if outpatient services are a good fit:
- Presence of a moderate to severe mental health condition that significantly impacts daily function.
- The ability to lead a generally stable life at home without 24-hour supervision and support.
- A need for structured treatment and routine.
- A safe and stable living environment that does not jeopardize an IOP’s effectiveness.
- A desire to participate, stay engaged, and grow.
Another common trigger for entry into an IOP is experiencing what’s known as a “first psychotic episode.” A first psychotic episode is simply the first time someone experiences the acute symptoms of psychosis like hallucinations, paranoia, delusions, and disorganized thinking. While these symptoms may have subsided somewhat since the initial episode, following up with entry into an IOP is an established and effective way to intervene and ultimately manage what may be serious mental health disorders.
Taking prompt action after a first psychotic episode allows providers and others within a mental health services administration to take action quickly, and assess and diagnose what may have triggered the episode. From there, they have the ability to prescribe medications for symptom management and gradually build and reinforce healthy lifelong habits through therapy sessions, which if adhered to can greatly limit the potential damage caused by untreated moderate to severe mental health disorders.
“An IOP provides a structured and supportive short-term intervention for someone who has experienced a psychotic episode,” Dr. Janssen says. “Providing symptom stabilization, identification of coping skills, relapse prevention planning, and getting resources in place for longer-term treatment will help them get back to previous activities like work or school.”
Taking the next step
Living–and thriving–with a moderate to severe mental illness is possible with the right support structure in place. Entering an intensive outpatient program, while no small step, is often the best option for getting that structure in place without committing to time in a residential psychiatric treatment facility. If you believe you or a loved one would benefit from an intensive outpatient program, the compassionate professionals at Ellie Mental Health can help guide you through your treatment options.
You can take that first step by learning more about Ellie’s IOPs here:


