All women go through a lot in their daily lives. From work stress to dealing with relationships and financial obligations to parenting and making sure the kids have everything they need – sometimes being a woman can be a complete roller coaster ride – the kind where you’re not sure if you’re going to make it to the end! And on top of it all, we also have to deal with our own bodily functions that sometimes can be just as difficult as everything else in our lives.
What are we talking about here? Not just that monthly visitor that we all would rather not hear knocking at the door (our periods), but PMS. Yes, that one. However, there is also another version of PMS, and this one can be much more severe and debilitating.
Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are two conditions that affect many women worldwide. Both PMS and PMDD are related to a woman’s menstrual cycle and can cause a variety of physical and emotional symptoms. However, there are some key differences between the two conditions that are important to understand.
Here, we’ll explore the differences between PMS and PMDD as well as the symptoms, causes, available treatments, and what you can do to cope.
Are severe symptoms of PMS or PMDD affecting your daily life? Reach out to Ellie Mental Health today to talk with a compassionate and qualified therapist.
Difference Between PMS and PMDD
Premenstrual syndrome (PMS) is a common condition that affects many women during their menstrual cycle. It typically occurs in the days or weeks leading up to a woman’s period and is thought to be caused by hormonal changes in the body.
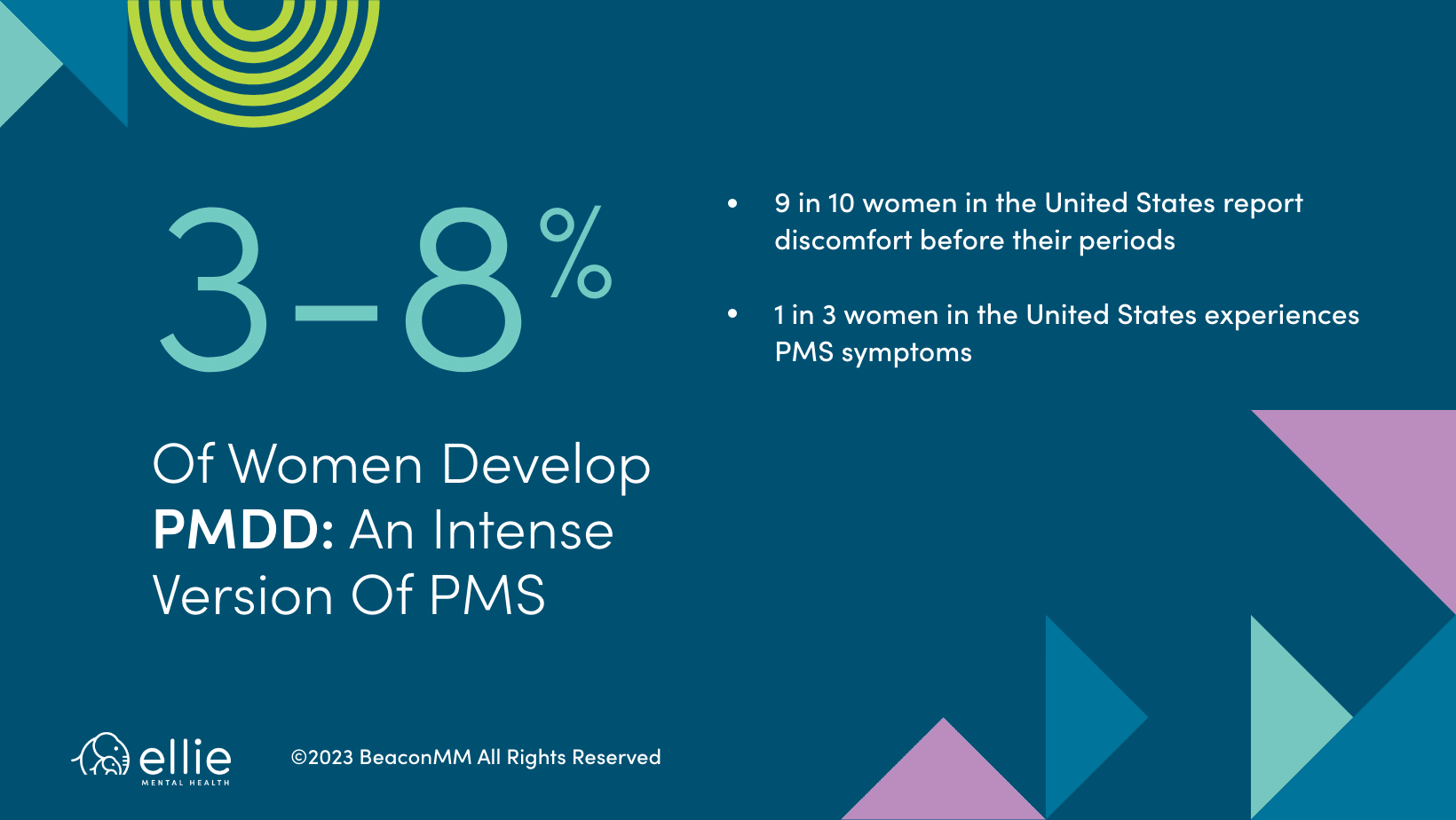
Premenstrual dysphoric disorder (PMDD) is a more severe form of PMS that affects around 3-8% of women. Although the symptoms of PMDD are similar to those of PMS, they are typically more severe and can significantly impact your daily life. PMDD is also caused by hormonal changes in the body, but the exact cause is not fully understood. In fact, some medical professionals have theorized that PMDD may be genetic. PMDD symptoms typically occur in the days leading up to a woman’s period and usually subside within a few days after the period begins. Though in some severe cases, PMDD can last for several weeks. And if this is the case, it is recommended that you see your healthcare provider as soon as possible.
PMS vs PMDD Symptoms
Let’s be real: periods can be a total pain. But if you’ve ever wondered why some months feel like a minor inconvenience and others like an emotional rollercoaster, you’re not alone. We’re diving into the nitty-gritty of the actual symptom differences between PMS and PMDD.
Symptoms of PMS
Physical symptoms of PMS include:
- Breast tenderness or swelling
- Bloating and water retention
- Headaches or migraines
- Fatigue or lack of energy
- Changes in appetite or food cravings
- Muscle aches and joint pain
Emotional symptoms of PMS include:
- Mood swings or irritability
- Anxiety or depression
- Difficulty sleeping
- Poor concentration or memory
- Changes in libido
Symptoms of PMDD
In addition to symptoms of PMS, someone with PMDD may also experience the following symptoms:
- Insomnia
- Feeling overwhelmed
- Suicidal thoughts or feelings
- Extreme changes in libido
While having some emotional ups and downs is normal with the hormonal changes that come with that time of the month, PMDD feels more intense and comes with more extreme changes in the week before and then disappear entirely a few days into your period. You might notice severe depressive symptoms, mood swings, and feeling like you’re on high alert.
How is PMDD Diagnosed?
The diagnosis of PMDD is typically based on the woman’s reported symptoms. If you are suspecting that you might be dealing with PMDD, a first step you could take is to see your primary care physician for hormonal testing. There’s no specific test for PMDD, but some blood tests can rule out other possible conditions that cause similar symptoms. After that, therapy can be an excellent way to learn tools and skills for coping with the emotional symptoms.
To diagnose PMDD, a woman typically must have at least five of the emotional and physical symptoms listed above, and these symptoms must occur only the week before her period starts. The symptoms must also be severe enough to interfere with her daily life.
What causes PMS and PMDD?
The exact cause of PMS and PMDD is not fully understood, but they are both thought to be caused by hormonal changes in the body. Specifically, PMS and PMDD are thought to be caused by fluctuations in estrogen and progesterone levels during the menstrual cycle.
However, there may be other factors that contribute to the development of PMS and PMDD, including:
- Genetics: There may be a genetic component to PMS and PMDD, as they tend to run in families.
- Brain chemistry: Some studies suggest that women with PMS and PMDD may have abnormal levels of certain neurotransmitters, such as serotonin.
- Environmental factors: Stress, poor diet, lack of exercise, and other environmental factors may contribute to the development of PMS and PMDD.
PMS and PMDD Treatments
The treatment of PMS and PMDD depends on the severity of the symptoms and how much they interfere with a woman’s daily life. The treatment for these conditions might include therapy, mental health medications, and recommended home care. In fact, many women report reduced symptoms after they alter their diets or implement stress-management activities.
A few home care methods for addressing symptoms of both PMS and PMDD include:
- Implementing healthy food choices
- Eliminating alcohol and caffeine
- Regular weekly exercise
- Heat therapy
- Stress management techniques (Yoga, meditation, Tai Chi)
- Proper sleep each night
- OTC medications such as Acetaminophen or Ibuprofen
It’s important to note that if you’ve been trying home remedies such as changing your diet and implementing stress-relieving activities and you’re still experiencing severe or debilitating symptoms, this is when it’s time to throw in the towel and see a medical professional.
While home care can be beneficial, some women have severe symptoms that may drastically alter their mental state. If conditions become severe, seeking out a therapist to talk to about your symptoms is highly recommended. For example, a therapist can work with you to help you manage mental health medications such as antidepressants and learn coping skills to manage symptoms of PMS/PMDD that may be affecting your mood and behavior.
The most common medications prescribed for PMDD are serotonin medications like SSRIs (Lexapro, Zoloft, Celexa, Prozac). Some people take SSRI medication continuously and find this helps best and others take it only for the weeks leading up to their period. One of our prescribers, Sara Polley, MD added: “I had a patient who normally takes 10mg Lexapro daily and then increases to 15mg daily for a week out of a month and feels this helps.”
SSRIs can be combined with hormonal contraceptive medications (birth control pills for example) that blunt the hormone changes during someone’s menstrual cycle. For some people, using birth control to skip their periods can be helpful, but for others this doesn’t make a difference.
Bottomline: There are many medication options available if you’re struggling with PMDD.
Some side effects of these medications can include changes in weight, libido, sleep changes, headaches, stomach upset – although these are rare and most people do not experience side effects with SSRI medication or hormonal contraceptive medications. We recommend reaching out to your prescriber if you notice any changes with your body or mood that are bothersome to discuss as they could be a side effect of your medication and your prescriber can discuss other options.
When Should I See a Therapist for PMS or PMDD?
At the end of the day, if your symptoms are significantly disrupting your daily life and making it difficult for you to get through simple tasks, a therapist can help direct you toward the best path of coping with your symptoms. And if therapy proves ineffective, a therapist may recommend that you see a gynecologist or other healthcare professional.
Mood swings, irritability, and poor concentration are a few symptoms that may make daily life difficult for those with severe PMS or PMDD. But when you begin withdrawing socially or begin having unprovoked moments of anger, thoughts of suicide, or other dark thoughts – don’t try to endure these symptoms alone.
At Ellie, we’re here to help guide you toward greater mental health. And sometimes, just talking about how you’re feeling can be the first step toward coping with your symptoms and getting the help that you need. Are you having difficulty coping with symptoms related to PMS or PMDD? Contact Ellie Mental Health today to speak with a compassionate and qualified therapist.


