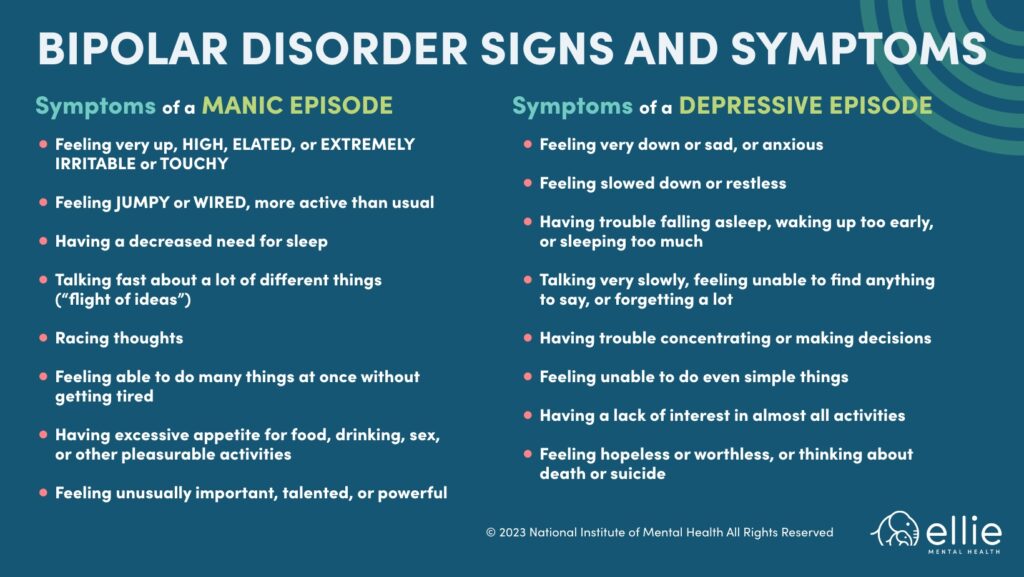
In some ways, Bipolar Disorder is a pretty straightforward mental illness and is fairly easy to diagnose (at least in theory): A person has a manic episode which, without treatment, can last anywhere from a few weeks to a few months. The manic episode is followed by a major depressive episode which, if left untreated, can go on for months or even years.
Despite what appears to be a clear-cut set of symptoms that occur in a predictable order, Bipolar Disorder (sometimes referred to as Manic Depression) is among the most frequently misdiagnosed mental health conditions, with some studies showing that at least 40% people with Bipolar Disorder initially get diagnosed with something else (usually Major Depressive Disorder or a Substance Use Disorder). Moreover, some research suggests that up to half of people initially diagnosed with Bipolar Disorder actually have something else going on instead. Why is that? What makes it so hard to get it right when it comes to diagnosing Bipolar Disorder?
The Difficulty in Diagnosing Bipolar Disorder
To understand why Bipolar Disorder so often gets misdiagnosed, it’s probably helpful to know a little bit about diagnosing mental illnesses in general. You see, unlike physical illnesses, such as cancer or Parkinson’s, mental illnesses are “constructs.” Meaning, you can’t run a blood test or an MRI and find irrefutable evidence that someone has a mental illness. The mental health conditions contained in the Diagnostic and Statistical Manual (the guidebook we use to make mental health and developmental diagnoses) were created by committees, based on observations and extensive research into clusters of symptoms that seem to show up together consistently. It is the best system we have come up with so far to identify and treat mental health conditions, but it is far from perfect.
One problem with this approach to diagnosing mental health conditions is that the human brain is far more complicated than other parts of the body. It has a tendency to create the same symptoms in response to any number of both psychological and physical problems. Bipolar Disorder, for example, shares symptoms with health conditions like a malfunctioning thyroid and multiple sclerosis. For example, someone with hyperthyroidism may develop insomnia, manic symptoms and may even experience hallucinations and delusions, all of which are also symptoms of a manic episode in someone with bipolar disorder. Certain medications can also “trigger” symptoms that look a lot like manic episodes. I personally learned that one the hard way when my then-5-year-old daughter was given a steroid medication to treat her asthma, and within just a few hours, I had a highly agitated Tasmanian Devil in my living room, spinning around in circles and talking about her plans to build an entire empire out of playing cards.
Diagnoses with Similar Symptoms as Bipolar Disorder
Another problem we run into when it comes to diagnosing is that many mental health conditions can look a lot like other mental health conditions. In other words, the lines between diagnostic categories can be quite blurry. And since there are no conclusive tests we can run to make sure we have the right diagnosis, there is usually some amount of guesswork involved, which means mistakes can – and do – get made.
With that as the backdrop, let’s now talk about some of the complications we might run into when diagnosing Bipolar Disorder. When it comes to misdiagnosing someone who actually has Bipolar Disorder, one of the most common reasons for this is because many people with Bipolar Disorder a) have not yet experienced a manic episode, so they have no reason to report symptoms of mania, or b) they don’t seek help until they experience a severe depressive episode, they fail to mention earlier symptoms of mania, and no one thinks to ask them about it. If the person doing the diagnosing only hears about depressive symptoms, they are probably going to give a diagnosis of Major Depressive Disorder. Unfortunately, the most common medications used to treat depression – specifically, selective serotonin reuptake inhibitors (commonly referred to as SSRIs), such as Prozac – can trigger manic episodes in people with Bipolar Disorder. Although far from ideal, an SSRI-induced manic episode is probably one of the most common paths to an accurate diagnosis of Bipolar.
Learn more about TMS therapy for treatment resistant depression.
Another complication in making an accurate diagnosis has to do with the high rate of substance use in people with Bipolar Disorder. Not to mention, someone experiencing a manic episode might look and sound a lot like someone who is high on stimulants or hallucinogens. Healthcare providers who aren’t trained in differentiating between drug use and mania might draw the wrong conclusion. Or if the person has both a Substance Use Disorder and undiagnosed Bipolar Disorder, the treatment team might focus on treating the substance use without realizing the person also has a serious underlying mental illness.
Bipolar Disorder also has a number of subtypes, and here is where the water gets really muddy. Bipolar I Disorder is the most straightforward: a full-blown manic episode, followed by a major depressive episode. But then we have Bipolar II Disorder, Cyclothymic Disorder, and Bipolar Disorder with “rapid cycling.” I will spare you a lecture on the specifics of each of these conditions, but suffice it to say that even those of us with extensive training in diagnosing mental health conditions can get tripped up when trying to tease apart these subtypes. Fortunately, mood stabilizers are the best line of treatment for most people with any of these disorders, which means that as long as we get the general category correct, the individual should be able to get the symptom relief they need with the right mood stabilizer, therapy, and social support.
In my experience, however, Bipolar Disorder too often gets misdiagnosed in individuals who present with extreme mood swings, but don’t actually have Bipolar Disorder or any of its subtypes. Specifically, I see a lot of people get diagnosed with Bipolar Disorder when the more accurate diagnosis is Borderline Personality Disorder. Even though Bipolar Disorder and Borderline Personality Disorder are believed to have completely different causes and treatments, they share enough common traits to confuse more than a few therapists and medical professionals. I suspect this is because individuals with Borderline Personality Disorder can be extremely moody, and they might even experience a level of energy and agitation that makes them seem “manic” to the people around them. Moreover, people with Borderline Personality Disorder often suffer from Major Depressive Disorder, which means their periods of high energy and agitation might be followed immediately by serious depressive symptoms, including suicidal thoughts and self-harm. Because the switch from “high” to “low” can be so abrupt, people assume they have Bipolar Disorder. But since the treatments for these two disorders are very different from each other, a misdiagnosis means the person isn’t going to get the right treatment, which can lead to unnecessary and prolonged suffering.
How Do I Get an Accurate Diagnosis?
The bottom line is that all of the mental health conditions I’ve mentioned here should only be diagnosed by a trained mental health professional. Although psychiatrists, and even general practitioners, can technically diagnose and treat both Bipolar Disorder and Borderline Personality Disorder, I personally believe the best way to ensure an accurate diagnosis is through a formal psychological assessment. Of course, psychologists make mistakes too, but because we receive more formal training in assessment and diagnosis than our mental health and medical counterparts, we are more familiar with the nuances between the different types of Bipolar Disorder, and a formal assessment will almost always make it clear whether the individual has bipolar disorder, borderline personality disorder, or a different condition altogether.
What is the Typical Treatment of Bipolar Disorder?
For Bipolar I Disorder, or one of its subtypes, the recommended treatment is usually medication, along with individual or group psychotherapy and maintaining a strong social support network. For Borderline Personality Disorder, Dialectical Behavioral Therapy (DBT) can be extremely effective, and it includes both group and individual therapy. Often, someone with Borderline Personality Disorder will also benefit from medication to treat their depressive symptoms, mood swings and agitation.
If you are experiencing extreme mood swings, with extreme highs and extreme lows, it is a good idea to talk with your therapist or healthcare provider about scheduling a psychological assessment. Living with extreme mood swings, whatever the cause, is exhausting and can wreak havoc on your life. Thankfully, there are effective treatments for Bipolar Disorder and Borderline Personality Disorder. An accurate diagnosis means you’ll receive the right treatment, right off the bat


